Glaucoma Treatment from Our San Francisco Eye Doctors
It is estimated that three million Americans have glaucoma, but only about half of them know that they have glaucoma. Glaucoma is a leading cause of blindness for people over 60 years old. But blindness from glaucoma can often be prevented with early treatment. When glaucoma develops, usually you don’t have any early symptoms and the disease progresses slowly. In this way, glaucoma can steal your sight very gradually. Fortunately, early detection and treatment (with glaucoma eyedrops, glaucoma surgery or both) can help preserve your vision.
The optic nerve is connected to the retina — a layer of light-sensitive tissue lining the inside of the eye — and is made up of many nerve fibers, like an electric cable is made up of many wires. The optic nerve sends signals from your retina to your brain, where these signals are interpreted as the images you see.
In a healthy eye, excess fluid leaves the eye through the drainage angle, keeping pressure stable.
In the healthy eye, a clear fluid called aqueous (pronounced AY-kwee-us) humor circulates inside the front portion of your eye. To maintain a constant healthy eye pressure, your eye continually produces a small amount of aqueous humor while an equal amount of this fluid flows out of your eye. If you have glaucoma, the aqueous humor does not flow out of the eye properly. Fluid pressure in the eye builds up and, over time, causes damage to the optic nerve fibers.
There are several types of glaucoma:
Open-angle glaucoma
Normal-tension glaucoma
Angle-closure glaucoma (also called "closed-angle glaucoma" or "narrow-angle glaucoma")
Congenital glaucoma
Secondary glaucoma
Glaucoma suspect
Glaucoma damage is permanent—it cannot be reversed. But medicine and surgery help to stop further damage.
What Does Glaucoma Look Like?
Click on the glaucoma vision simulator link below to see what it’s like to develop glaucoma.
Glaucoma Treatment
Medicated eye drops are the most common way to treat glaucoma. These medications lower your eye pressure in one of two ways — either by reducing the amount of fluid created in the eye or by helping this fluid flow out of the eye through the drainage angle.
These eyedrops must be taken every day. Just like any other medication, it is important to take your eyedrops regularly as prescribed by your ophthalmologist.
Once you are taking medications for glaucoma, your ophthalmologist will want to see you regularly. You can expect to visit your ophthalmologist about every 3–6 months. However, this can vary depending on your treatment needs.
If you have glaucoma, it is important to tell your ophthalmologist about your other medical conditions and all other medications you currently take. Bring a list of your medications with you to your eye appointment. Also tell your primary care doctor and any other doctors caring for you what glaucoma medication you take.
Types of Glaucoma Surgery
In some patients with glaucoma, surgery is recommended. Glaucoma surgery improves the flow of fluid out of the eye, resulting in lower eye pressure.
Laser trabeculoplasty
A surgery called laser trabeculoplasty is often used to treat open-angle glaucoma. There are two types of trabeculoplasty surgery: argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT).
During ALT surgery, a laser makes tiny, evenly spaced burns in the trabecular meshwork. The laser does not create new drainage holes, but rather stimulates the drain to work better.
SLT uses a newer, lower-energy laser which only treats specific cells in the drainage angle. SLT and ALT are equally good at lowering eye pressure.
Even if laser trabeculoplasty is successful, most patients continue taking glaucoma medications after surgery. For many, this surgery is not a permanent solution. Nearly half of the people who receive this surgery develop increased eye pressure again within five years. Many people who have had a successful laser trabeculoplasty will need more treatment in the future. This treatment may be another laser, more medication or surgery.
Laser trabeculoplasty can also be used as a first line of treatment for patients who are unwilling or unable to use glaucoma eye drops.
Laser iridotomy
Laser iridotomy is recommended for treating people with closed-angle glaucoma and those with very narrow drainage angles. A laser creates a small hole about the size of a pinhead through the iris to improve the flow of aqueous fluid to the drainage angle.
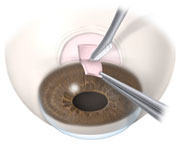
Trabeculectomy
In trabeculectomy, a flap is first created in the sclera (the white part of the eye). Then a small opening is made into the eye to release fluid from the eye.
In trabeculectomy, a small flap is made in the sclera (the outer white coating of your eye). A filtration bleb, or reservoir, is created under the conjunctiva — the thin, filmy membrane that covers the white part of your eye. Once created, the bleb looks like a bump or blister on the white part of the eye above the iris, but the upper eyelid usually covers it. The aqueous humor can now drain through the flap made in the sclera and collect in the bleb, where the fluid will be absorbed into blood vessels around the eye.
Eye pressure is effectively controlled in three out of four people who have trabeculectomy. Although regular follow-up visits with your doctor are still necessary, many patients no longer need to use eye drops. If the new drainage channel closes or too much fluid begins to drain from the eye, additional surgery may be needed.
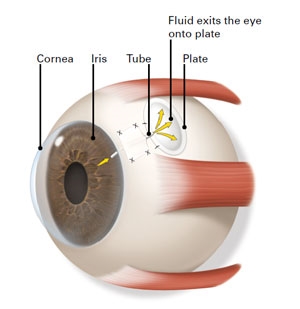
AQUEOUS SHUNT SURGERY
If trabeculectomy cannot be performed, aqueous shunt surgery is usually successful in lowering eye pressure.
A glaucoma drainage implant creates a new way for aqueous fluids to drain from the eye.
An aqueous shunt, or glaucoma drainage device, is a small plastic tube or valve connected to a reservoir (a roundish or oval plate). The plate is placed on the outside of the eye beneath the conjunctiva (the thin membrane that covers the inside of your eyelids and the white part of your eye). The tube is placed into the eye through a tiny incision and allows aqueous humor to flow through the tube to the plate. The fluid is then absorbed into the blood vessels. When healed, the reservoir is not easily seen unless you look downward and lift your eyelid.
Information courtesy of EyeSmart (geteyesmart.org).